Since remodeling serves both the structural and metabolic functions of the skeleton, it can be stimulated both by the hormones that regulate mineral metabolism and by mechanical loads and local damage acting through local factors. Repair of local damage is an important function of remodeling.
Which of the following factors affect bone remodeling and growth?
Bone growth factors affect the process of bone remodeling. These factors include insulin-like growth factors I and II, transforming growth factor beta, fibroblast growth factor, platelet-derived growth factor, and bone morphogenetic proteins. Bone volume is determined by the rates of bone formation and bone resorption.
What is the continual renewal and recycling of the bone matrix?
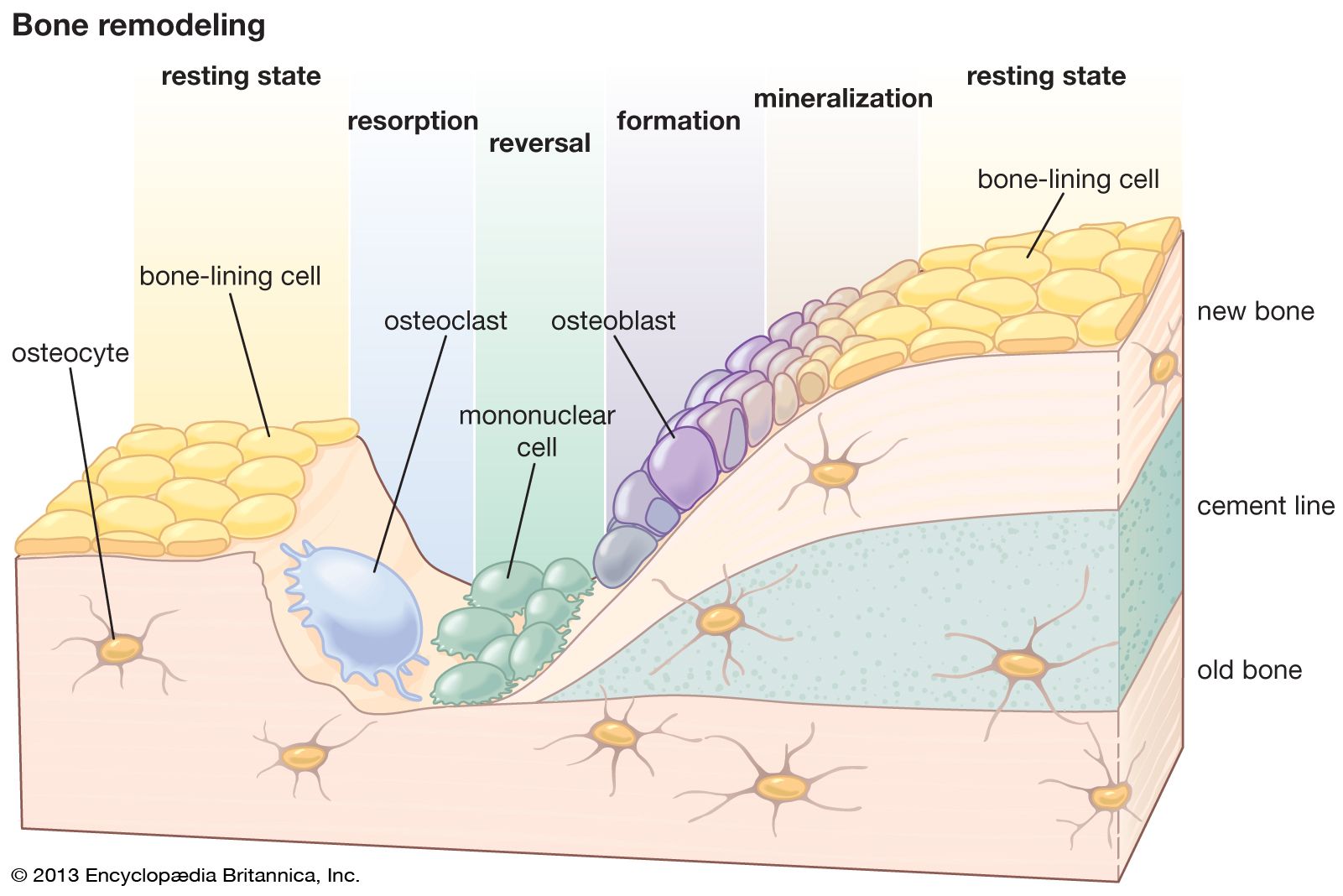
The skeleton is a metabolically active organ that undergoes continuous remodeling throughout life. Bone remodeling involves the removal of mineralized bone by osteoclasts followed by the formation of bone matrix through the osteoblasts that subsequently become mineralized.
Which of the following causes bone matrix resorption during bone growth and remodeling?
Bone tissue is continuously remodeled through the concerted actions of bone cells, which include bone resorption by osteoclasts and bone formation by osteoblasts, whereas osteocytes act as mechanosensors and orchestrators of the bone remodeling process.
What is a potential problem that can arise from the continual remodeling of bone matrix quizlet?
What is a potential problem that can arise from the continual remodeling of bone matrix? incorporation of heavy metals into the bone matrix.
What two factors cause bone to remodel?
Bone remodeling is the result of two opposite activities, the production of new bone matrix by osteoblasts and the destruction of old bone by osteoclasts.
What are the principles of bone Remodelling?
Bone remodeling occurs when healthy bone is renewed to maintain bone strength and maintain calcium and phosphate homeostasis. It proceeds through four phases: (1) cell activation, (2) resorption, (3) reversal, and (4) bone formation. Bone healing, on the other hand, involves rebuilding bone following a fracture.
Frequently Asked Questions
What are the two types of bone remodeling?
In adults, remodeling proceeds at about 10% per year. An imbalance in the regulation of bone remodeling's two sub-processes, bone resorption and bone formation, results in many metabolic bone diseases, such as osteoporosis.
What is bone remodelling regulated by?
The regulation of bone remodeling is both systemic and local. The major systemic regulators include parathyroid hormone (PTH), calcitriol, and other hormones such as growth hormone, glucocorticoids, thyroid hormones, and sex hormones.
What controls bone remodeling?
Bone remodeling is thought to be regulated by many factors including nutritional status, humoral factors, and biomechanical stress. However, the involvement of the autonomic nervous system, mainly the sympathetic nervous system (SNS), in the modulation of bone remodeling is beginning to receive more attention.
Which law states that bones remodel due to demands on the bone?
Wolff's Law is the idea that natural healthy bones will adapt and change to adapt to the stress that it is subjected to. For example, if the bones are subjected to heavier and heavier loads, they will naturally reconstruct themselves to accommodate that weight. This is how bones typically respond to stress.
What is the regulation of bone remodeling?
The regulation of bone remodeling is both systemic and local. The major systemic regulators include parathyroid hormone (PTH), calcitriol, and other hormones such as growth hormone, glucocorticoids, thyroid hormones, and sex hormones.
What is the law of bone in anatomy?
The premise that bones grow and remodel throughout life to adapt to their mechanical environment is often called Wolff's law. Wolff's law, however, is not always true, and in fact comprises a variety of different processes that are best considered separately.
What does the Wolff's law state?
This effect is called Wolff's Law. It states that our bones become thicker and stronger over time to resist forces placed upon them and thinner and weaker if there are no forces to act against. This principle is important for preventing injuries. A thicker bone is harder to break.
What is the significance of bone remodeling in calcium homeostasis?
Bone remodeling serves to adjust bone architecture to meet changing mechanical needs and it helps to repair microdamages in bone matrix preventing the accumulation of old bone. It also plays an important role in maintaining plasma calcium homeostasis. The regulation of bone remodeling is both systemic and local.
How does bone remodeling affect homeostasis of bone tissue?
Bone remodeling is essential for adult bone homeostasis. It comprises two phases: bone formation and resorption. The balance between the two phases is crucial for sustaining bone mass and systemic mineral homeostasis.
How bones are remodeled in response to low blood calcium ion levels?
The parathyroid hormone (PTH), secreted by the parathyroid glands, is responsible for regulating blood calcium levels; it is released whenever blood calcium levels are low. PTH increases blood calcium levels by stimulating osteoclasts, which break down bone to release calcium into the blood stream.
How do bone cells help maintain homeostasis?
The skeletal system helps maintain mineral homeostasis by regulating the level of calcium and other minerals in the blood by storing or releasing them from bones as needed. This process also helps maintain homeostasis in blood pH because the minerals are basic.
Does bone remodeling maintain blood calcium levels?
Bones are not inert structures within the human body; they continue to change over the course of a lifespan. This process of skeletal change is known as bone remodeling, which both protects the structural integrity of the skeletal system and metabolically contributes to the body's balance of calcium and phosphorus.
How does remodeling change bone structure in response to light and heavy stress?
What is the relationship between bone remodeling and stress?
FAQ
- What is the effect on bone in response to stress?
Stress alters the levels of growth hormones by modifying the HPA axis, growth hormone-releasing hormones, and growth hormone-inhibiting hormones. When this balance is upset by chronic stress, a decrease in growth hormones can develop, leading to bone loss.
- What is remodeling and how does it affect bone tissue?
This process of skeletal change is known as bone remodeling, which both protects the structural integrity of the skeletal system and metabolically contributes to the body's balance of calcium and phosphorus. Remodeling entails the resorption of old or damaged bone, followed by the deposition of new bone material.
- How does stress on muscles affect bone remodeling?
Exercise and Bone Tissue
Similarly, mechanical stress stimulates the deposition of mineral salts and collagen fibers. The internal and external structure of a bone will change as stress increases or decreases so that the bone is an ideal size and weight for the amount of activity it endures.
- Which bone cells are responsible for destroying old bones?
- Osteoclasts are involved in bone resorption that contributes to bone remodelling in response to growth or changing mechanical stresses upon the skeleton. Osteoclasts also participate in the long-term maintenance of blood calcium homeostasis.
- What is responsible for breaking down bone during remodeling?
- Osteoclasts dissolve and break down old or damaged bone cells. They make space for osteoblasts to create new bone tissue in areas that are growing or need repair. If osteoblasts are builders, osteoclasts are your bones' demolition crew.
- What is the process of destroying old bone?
The osteoclasts remove bone by dissolving the mineral and breaking down the matrix in a process that is called bone resorption. The osteoclasts come from the same precursor cells in the bone marrow that produce white blood cells.
- What is responsible for Bone Remodelling?
As already mentioned, two principal bone cells actively attend the bone remodelling, that is the osteoblasts and the osteoclasts, and an overview of their regulation and function will be done.
- Do osteoblasts break down old bone?
Osteoblasts, osteocytes and osteoclasts are the three cell types involved in the development, growth and remodeling of bones. Osteoblasts are bone-forming cells, osteocytes are mature bone cells and osteoclasts break down and reabsorb bone.
- What is a potential problem that can arise from the continual remodeling of bone matrix
What is a potential problem that can arise from the continual remodeling of bone matrix? Incorporation of heavy metals into the bone matrix. What is the
- How will you describe bone remodeling?
The skeleton is a metabolically active organ that undergoes continuous remodeling throughout life. Bone remodeling involves the removal of mineralized bone by osteoclasts followed by the formation of bone matrix through the osteoblasts that subsequently become mineralized.
- What is bone remodeling characterized by?
Bone remodelling is an active and dynamic process that relies on the correct balance between bone resorption by osteoclasts and bone deposition by osteoblasts.
- What is the physiology of bone remodeling?
This process of skeletal change is known as bone remodeling, which both protects the structural integrity of the skeletal system and metabolically contributes to the body's balance of calcium and phosphorus. Remodeling entails the resorption of old or damaged bone, followed by the deposition of new bone material.
- What are the 4 steps to bone remodeling?
- Following the fracture, secondary healing begins, which consists of four steps:
- Hematoma formation.
- Granulation tissue formation.
- Bony callus formation.
- Bone remodeling.
What is a potential problem that can arise from the continual remodeling of bone matrix?
| What is an example of bone remodeling? | For example, in response to weight training, “loading” of bone will trigger osteoclasts and osteoblasts to reorganize bone matrix in the direction of force and increase bone density. Also, after a long-bone fracture, osteoblasts lay down new bone as the final step in the healing cascade. |
| What is bone Remodelling turnover? | Bone turnover (remodelling) Bone turnover is the process of resorption followed by replacement by new bone with little change in shape, and it occurs throughout a person's life. Osteoclasts break down bone (bone resorption), releasing the minerals, resulting in a transfer of calcium from bone fluid to the blood. |
| What is the active turnover of bone? | Bone turnover markers (BTMs) are biochemical products of bone remodeling that can be measured usually in blood or urine. They reflect the metabolic activity of bone but have no function in controlling skeletal metabolism. They are traditionally categorized as markers of bone resorption and markers of bone formation. |
| Why does bone need to turnover or remodel? | Bones are not inert structures within the human body; they continue to change over the course of a lifespan. This process of skeletal change is known as bone remodeling, which both protects the structural integrity of the skeletal system and metabolically contributes to the body's balance of calcium and phosphorus. |
| What is normal bone turnover? | The relatively low adult cortical bone turnover rate of 2 to 3%/yr is adequate to maintain biomechanical strength of bone. The rate of trabecular bone turnover is higher, more than required for maintenance of mechanical strength, indicating that trabecular bone turnover is more important for mineral metabolism. |
| Is bone turnover same as remodeling? | Bone remodelling is a cellular mechanism behind the bone turnover. It renews the old bone piece by piece and thus ensures the correction of possible microdamage and enables the regulation of mineral homeostasis. |
| What is the law of transformation of bone? | What is Wolff's Law? Wolff's Law is the idea that natural healthy bones will adapt and change to adapt to the stress that it is subjected to. For example, if the bones are subjected to heavier and heavier loads, they will naturally reconstruct themselves to accommodate that weight. |
| What forces are bone remodeling? | Mechanical forces play essential roles in bone remodeling. Mechanical cyclical stretching (MCS), fluid shear stress (FSS), compression, and microgravity play different roles in cell differentiation and proliferation by affecting intracellular interactions. |
| What is bone Remodelling theory? | Bones are not inert structures within the human body; they continue to change over the course of a lifespan. This process of skeletal change is known as bone remodeling, which both protects the structural integrity of the skeletal system and metabolically contributes to the body's balance of calcium and phosphorus. |
| What is expansile remodeling of bone | By B Langdahl · 2016 · Cited by 384 — Bone modeling describes the process whereby bones are shaped or reshaped by the independent action of osteoblast and osteoclasts. The activities |
| What is bone remodeling controlled by? | The regulation of bone remodeling is both systemic and local. The major systemic regulators include parathyroid hormone (PTH), calcitriol, and other hormones such as growth hormone, glucocorticoids, thyroid hormones, and sex hormones. |
| Which system controls bone remodeling? | Autonomic nervous system The sympathetic neural pathway is so far the only identified link between the potent leptin-dependent central control and bone cells. An intact autonomic nervous system contributes to the maintenance of healthy bone tissue. Conversely, disturbance of the autonomic nervous system could induce abnormal bone remodeling. |
| What directly controls bone remodeling? | Bone remodeling is thought to be regulated by many factors including nutritional status, humoral factors, and biomechanical stress. However, the involvement of the autonomic nervous system, mainly the sympathetic nervous system (SNS), in the modulation of bone remodeling is beginning to receive more attention. |
- Which controls bone remodeling quizlet?
The hormone that is primarily involved in the control of bone remodeling is the parathyroid hormone.
- How do osteocytes regulate bone remodeling?
Osteocytes regulate bone formation through sost/sclerostin. Thus, bone formation induced by systemic elevation of PTH or local mechanical loading is associated with decreased expression of sclerostin. Osteocytes regulate bone resorption through pro- and anti-osteoclastogenic cytokines.
- What does Wolff's law of bone state?
This effect is called Wolff's Law. It states that our bones become thicker and stronger over time to resist forces placed upon them and thinner and weaker if there are no forces to act against. This principle is important for preventing injuries. A thicker bone is harder to break.
- What is bone remodeling quizlet?
Bone remodeling (or bone metabolism) is a lifelong process where mature bone tissue is removed from the skeleton (a process called bone resorption) and new bone tissue is formed (a process called ossification or new bone formation).
- What is the role of calcium in bone Remodelling?
- Destruction, or resorption, of bone by large cells called osteoclasts releases calcium into the bloodstream to meet the body's metabolic needs and simultaneously allows the bone—which is inhibited by its inorganic component from growing by cell division like other tissues—to alter size and shape as it grows to adult
- What is the role of calcium in bones explain?
Calcium is a mineral your body needs to build and maintain strong bones and to carry out many important functions. Calcium is the most abundant mineral in the body. Almost all calcium in the body is stored in bones and teeth, giving them structure and hardness.
- What stimulates bone remodeling?
The regulation of bone remodeling is both systemic and local. The major systemic regulators include parathyroid hormone (PTH), calcitriol, and other hormones such as growth hormone, glucocorticoids, thyroid hormones, and sex hormones.
- What role do hormones play in bone remodeling and regulation of calcium in the blood?
Three calcium-regulating hormones play an important role in producing healthy bone: 1) parathyroid hormone or PTH, which maintains the level of calcium and stimulates both resorption and formation of bone; 2) calcitriol, the hormone derived from vitamin D, which stimulates the intestines to absorb enough calcium and
- Is calcium needed for bone healing?
- Calcium and vitamin D are nutrients associated with healthy bones, so if you have a broken bone, a stress fracture or have had a joint replacement, make sure to get plenty of these nutrients to strengthen your bones. The best sources of calcium and vitamin D are low-fat dairy foods.
- What is involved in bone remodeling?
Bone remodeling involves the removal of mineralized bone by osteoclasts followed by the formation of bone matrix through the osteoblasts that subsequently become mineralized.
- What are the 2 main hormones in bone remodeling?
Three calcium-regulating hormones play an important role in producing healthy bone: 1) parathyroid hormone or PTH, which maintains the level of calcium and stimulates both resorption and formation of bone; 2) calcitriol, the hormone derived from vitamin D, which stimulates the intestines to absorb enough calcium and
- What is the main ion in bone?
The inorganic material of bone consists predominantly of phosphate and calcium ions; however, significant amounts of bicarbonate, sodium, potassium, citrate, magnesium, carbonate, fluorite, zinc, barium, and strontium are also present [1, 2].
- What are the 3 main things that affect bone remodeling?
Bone remodeling is thought to be regulated by many factors including nutritional status, humoral factors, and biomechanical stress. However, the involvement of the autonomic nervous system, mainly the sympathetic nervous system (SNS), in the modulation of bone remodeling is beginning to receive more attention.